Find the nearest provider of the O-Shot® combined with an Emsella treatment<--
Physicians apply for training to provide the O-Shot® procedure<--
Transcript (References at the bottom of the page).
You can lift the hood of your car, and you can name the parts: There's the carburetor, there's the radiator. You can take off the cover of your computer and say there's the integrated circuit, that's a diode, that's a resistor, that's a wire, but that doesn't mean you know how those parts work together to make your computer do what it does. So your computer is a system with components that work together, and then there are systems within the systems.
The body is also a system with subsystems within it: the respiratory system, the pulmonary system, and the orgasm system. And we're talking about how the muscles of the pelvis contribute not to urinary continence but to sexual function, not incontinence to sexual function.
The idea is to not only lift the hood of the pelvis and name parts but also to understand how the parts (including the muscles) work together as a system to contribute to sexual function and orgasm (and look at the research that supports understanding of the system).
In previous lessons, we reviewed the hidden clitoris. The hidden lies in intimate proximity with the sex muscles—which is the subject of the rest of this lesson.
From the top and from the bottom
This is the pelvic floor, but there's more to the pelvic muscles than the pelvic floor.

Notice that you can see muscles from the caudal side that you don't see on the cephalad side: caudally, you see superficial transverse perineal muscle, deep transverse perineal muscle, ischiocavernosus, and bulbospongiosus.
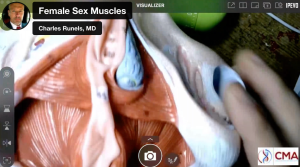
Those are not part of the pelvic floor. Some think every muscle in the female pelvis is part of the pelvic floor. But, every muscle in the female pelvis is absolutely not part of the pelvic floor.
Here, you’re seeing the caudal view of the floor where you have puborectalis, iliococcygeus, ischiococcygeal, and coccygeus. So those three together, these first three form the levator ani.
And you can see how if these contract, it's going to pull the anus up, levator ani.
Well, let me pull out the other model because I think it makes it more apparent for you. Okay, so this model has some of the organs in place. We’re going to take out the ovaries, the fallopian tubes, and the uterus. But of course, the vagina has at least muscle cells in it. And so we'll put that aside for now. And then, let's take out the bladder, which has a muscular layer and urethra.
The urethra, or the urinary sphincter, has three layers: two layers of striated muscle and one layer of smooth muscle.
And some of those layers go circumferentially around both the vagina, so it sits like that. And so some of the muscles go that are more distal from the bladder go circumferentially around both the urethra and the vagina.
And then as you get more proximal to the bladder, they just go part of the way. And then you have muscles that go around just the urethra, both circumferentially and longitudinal. But those are, I think, more easy to understand what they do. Now, we have the pelvic floor exposed, and you can look through; this is called the hiatus.
Wait, let's pull out the rectum. Okay, so now you have holes in the pelvic floor. You need them, right? So you need a hole for, if you look at the other side, it makes sense, you need a hole for the rectum, hole for the vagina, hole for the urethra. And those would be the hiatus or the absence of the pelvic floor muscles.
So you have puborectalis that comes down. And let's pull it this way so you can see it better. I'll hold it more still. So you got puborectalis right there. Pubococcygeus comes down right there, iliococcygeus, ischiococcygeus or coccygeus, all of these forming the floor. But look what happens. Now, there's in reality, in the women, of course these muscles are adjacent to each other. And if you look at the other model, it demonstrates ... thanks to my amazing wife, I've talked to her about what it's like to be down there doing surgery and got some of these ideas from her ... but there's not a lot of space right there. And dissecting the deep, transverse perineal muscle away from the pelvic floor would be difficult because they’re abut each other; they touch but have different fibers and different functionalities, which we’re getting to, and how they relate to the sexual function.
So, let’s look back at the pelvic floor. And here's a question to ask yourself:
If you go with the assumption that there is no redundancy and no wasted parts in the body and we want to care for a woman, then we should we not understand every one of these muscles, where they attach and what they do to contribute to sexual function and orgasm?
I do this all the time: I put together stairs for our hot tub the other day, and I had an extra part, which bothered me. I don't think people build something as simple as a do-it-yourself kit for making stairs and throw in extra parts.
So, I don’t think we should look at any part of the woman’s pelvis, including every one of the muscles in her pelvis, and just assume parts of it do not matter—as if the parts we don’t understand are just extra and do not matter.
I guess you could argue that maybe the appendix is an extra part, but not really because it's vestigial, and it’s a part that, because it’s extra, sort of dried up, you might say, or become pygmy size. So if you go with that assumption, there are no extra parts, and every part has a function, then consider this: it is easy to imagine what the bicep muscle does, right? There’s a hinge across our midway in the bicep muscle, and when it contracts, it's easy to see what it does. It brings the radius closer to the humerus, and your elbow acts like a hinge.
Why is the pelvic floor made of muscle and not of tendons?
But if the floor is meant just to hold things in place within the pelvis, why is it a muscle? Why isn't it just fascia, a thick fascial plane, or a tendon or something?
Why was it made to contract and relax?
I think that's a question worth asking. And it gets even more interesting, I think. We'll get to the research shortly, but I think the research makes more sense if you look at the functionality.
So, now with our model, we've lifted away from the pelvic floor, other muscles, and these are the ones I call the sex muscles because they might contribute to, of course, the anus would contribute to fecal continence. But you could argue the ischiocavernosus isn't doing anything for urinary continence, as far as I can see.
But now, let's name them again, and think about, well when it contracts if there are no extra parts and everything has a purpose, what's the purpose of this muscle contracting?
There's no joint. This is why I wanted to cover the mystery of the hidden clitoris before we got to the muscle part of the female orgasm system. It's just so amazingly beautifully designed. I think many of our colleagues just still think of the female genitalia as a tube to put a penis in and to push a baby out of.
There's also a tube for feces to come out of and a tube for urine to come out of. And they're not visualizing everything you're looking at here, but let's think about it.
Okay, (referring to model, see the video), so you've got labia majora, labia minora, urethra, vagina. Then, remember, the root of the clitoris is just above the urethra, and it's all attached. So you've got corpus cavernosi. I never know how to say the word crux. Is that crus or cuss or crux or I don't know what it is, but if you were to say it, I guess say it loudly, so I'm going to call it crus or I think it's crux, but whatever, corpus cavernosi. So you have two of them that lay along the pubic rami and the ischiocavernosus covers them.
And then you have the corpus spongiosus, also part of the clitoris and attached to the root, which is attached to the underbelly of the body of the clitoris. And then you have the glands, clitoris, and that little pink thing right there is Bartholin's gland.
Now think about this: What's the purpose of corpus spongiosus and ischiocavernosus and what's the purpose of transverse peroneal, deep transverse peroneal, superficial and peroneal body?
Even if you can name them, so what, how does it help you have better sex?!
Are we just making a more enjoyable place for a man’s penis?
Sex as a female is both for your pleasure and for your psychology, right, because it's not just about sexual pleasure. I'm not going to start ranting about that, but never forget sexual pleasure is not just about pleasure in the bedroom. It has been studied over and over again that somewhere between 30 and 40% of women have psychological distress because of sexual dysfunction.
Have you ever had a cracked window in a nice car? You don’t really need it fixed; it's not leaking water, but it bugs you.
Now, imagine you have a dysfunctional vagina. Even if you're not using it with your husband, it still bugs you. Even if you don't want a man in your house, it might still bother you because you want to make love to yourself.
So I know that's a sidetrack, but I just never want to forget, this is not just about pleasure, although it is, it's not just about pleasure, it's not just about making babies, although it is, because what brings pleasure to the woman is going to bring pleasure to the man if this is designed properly.
Think about it. If this is designed properly, this is going to make the man orgasm or ejaculate. So if he wants to again, if we're looking at it from propagation of the species, from a Darwinian standpoint, then you want this little device to make the man ejaculate. And then because it feels so good, he's going to want to ejaculate again in a few minutes from now and increase the chances of survival of the species.
And then if it feels good to the woman, even if he's in refractory period, if you're living in a cave somewhere where you haven't yet been exposed to modern mores and religious rules, she might want to have sex with his friend because it felt so good to her.
Watch the feral pussycat in your backyard; she’ll have tomcats lined up back to back, and you know she enjoys it because she does not run away between tomcats.
Some people say, "Well, you're talking about the vagina; you’re pushing for it to be tighter so it feels better to men."
Oh, no, no, no. Sometimes, tighter isn't better for a man. We never say tighter, loose, looser, big, or small; we talk about fit.
Does it fit?
The man loses about 50% of the endothelium of his penis by the time he's 65. So his penis is shrinking. Now, imagine a woman who has delivered several babies; think about what happens to this device (the female sex muscles and the pelvic floor muscles) when she delivers a child.
I'm just sidetracked, but I just wanted to put this in perspective about why we are talking about this. There's the propagation of the species perspective; there’s a pleasure to the man. Don't deny it because that's necessary for the propagation of the species (and for deepening relationships). And then there's also pleasure for the woman, both physical and psychological pleasure for both.
And most of your colleagues, if you're a physician, can't name all these parts.
Not all muscles connect to bone
All right, so here we go. Perineal body or the superficial transverse perineal muscle, deep transverse perineal muscle, bulbospongiosus, ischiocavernosus. And there are no joints associated with those muscles. To help understand muscles without joints, consider the face: the only muscle I know that is not attached to any bone at all is orbicularis oris muscle.1 The orbicular oris muscle does not connect to a bone, it connects to muscles only.
The perineal body is similar to the orbicularis oris in that it IS the connection of multiple muscles—it connects muscle to muscle.
And then you think, okay, what's it doing (the prineal body)?
When the muscles connecting to it contract, there’s no joint movement; there is not joint. And I don't yet have an answer that satisfies me, but here’s what I think is happening: both in men and women, the parasympathetic system causes erection and blood flow in the clitoris. Then, with ejaculation in men and with orgasm in women, you have contraction of the muscles we are discussing.
To understand something, I like to imagine the extremes. So if these muscles became extremely relaxed, like a worn-out rubber band. If all these muscles became like that, superficial transverse peroneal muscle and deep, transverse perineal muscle, if it became relaxed, so there was no tensile strength at all to it, well then with sex, this is not attached to a bone, the introitus is just free-floating, right? Of course, there are tendons on the other side, but this is mostly free-floating.
So when this (see video) becomes contractile, it helps hold the vagina in place. And then when the corpus spongiosum and the ischiocavernosus contract, it would squeeze blood flow, rhythmically if there was orgasm going on, from the corpus cavernosi up into the body and the glands, causing congestion and increased arousal.
And so there's a positive feedback loop.
You're aroused, you have an orgasm, and then with the contractions, there becomes even more arousal, more pleasure. And so you want to play again, and eventually, you make a baby, or you make a deeper, more interesting relationship with your lover.
Okay, so I'm calling these the female sex muscles.
Making things better
Remember one of the studies we looked at involving the clitoris? Even though the clitoris has the most nerve fibers, their understanding, Dr. Paul's, if you remember, was that the root was the most arousing. Now, think about that.
That coincides with Dr. Gräfenberg's idea about the urethra, which eventually evolved into the G-spot named after Dr. Gräfenberg. Let me explain:
If you go just inside the introitus and push up (anteriorly), you are then putting pressure on both the urethra and the clitoral root. Now, once you get past these muscles, what I'm calling the sex muscles, into the vagina itself, the strength goes down (more proximal, towards the cervix), you no longer have the circumferential overlay of the female sex muscles), nor the pubic symphysis anteriorly. Posteriorly, there is only the perineal body and no bone, so when you progress proximally and pass the perineal body, the vaginal wall becomes more mobile.
Relating male masturbation to the female sex muscles
Now, watch a man when he masturbates: There is an increased pleasure if there's a wave of compression. In other words, there may be more compression on one part of the penis, and then that compression moves up and down along the corpus cavernosi, which is exactly what would happen if the female sex muscles were contracting as the penis goes in and out.
In other words, if the introitus was tighter than what's going on inside the vagina. Okay, let's look at the research. Some of that was me going by common sense. Some of it was based on research. Some of it I might've just made up because it sounded good, but I think most of what I said was right.
Relevant William Osler
Remember what William Ocer said?
He said, “If I ask three medical students how long it takes for the fingernail to grow, one will not give it a second thought, another will look it up in the book, and the third will take a silver nitrate stick and put a mark at the base of their fingernail and see how long it takes to grow to the end."
So I think I'm dealing without those students here on this call. We're all students trying to understand what has not been explained adequately and what deserves much more research because the best answers have not yet been found—not even the best questions have been asked.
Okay, let's look at some of that research, and then I'll talk about some of the actual things we have, the technologies and ideas we have to make these muscles work better and deal with the dysfunction that might happen.
How to catch a bird with your hands (and how it relates to the pelvic floor)
My grandmother used to have a saying I was reminded of when I read the research we are about to discuss.
She was a sweet lady who was a little quirky. She had a Jesus picture on every wall, but never went to church unless somebody got married or died. And she's the only person I ever knew in my entire life who I never heard say anything bad about anybody—nobody else I can say that about.
And she used to tell me, "Charles, if you go outside and you sprinkle a little salt on a bird's tail, it won't be able to fly away, and you can catch it with your hands.”
If you think about that, it's the old catch-22, right? Because if you’re close enough to put salt on the bird’s tail, well, you are close enough to catch it without the salt. But, since you can’t get close enough to put the salt, you cannot use the method to catch a bird. So, you could drive yourself insane trying to take that advice (a pretty funny joke to the 5-year-old I was when she told me the method).
The following study reminded me of what my grandmother used to tell me. What they did was they took women and had them do a Kegel. They did bi-digital palpation, so two fingers, the index and the middle finger—they even said which fingers, into the vaginal introitus, about four centimeters in.
So you go four centimeters in or a little bit less than two inches. And then, they instruct the woman to squeeze their levator and anal muscles without activating other groups of muscles. In other words, you can't contract your gluteal muscles, your legs or your abdomen.
Then they palpated the pubococcygeus on each side of the vagina and said, "Do a maximal contraction of the pubococcygeus."
Okay, now they scored the strength of the contraction.
I'm getting to the part about the salt on the tail of the bird; promise it relates.
So then they scored it from a grade zero, no contraction, grade one minor flicker, grade two is a weak muscle contraction, grade three, they're only really starting to feel it, grade four is good, and then grade five is strong. So, grades one through five and zero are nothing. One's a flicker. Not until you get to three do you have something happening.
And if you look at what they snuck in on you—they defined that one muscle, the pubococcygeal muscle, with the pelvic floor muscles. And as you just saw, really is a lot more there, but okay, it's a good way to approximate. It's easy to reach with your finger, easy to identify, you just put your finger in the vagina, feel over to either side and that's it.
Now, here's the fun part. When they graded them on the female sexual function index. I love this study. They looked at it, and they saw, as you would expect, that those with stronger muscles had better sex.
But here's the part about the salt on the tail. Now, what do you do with that?
Here's the catch-22. If you have a weak contraction—nothing or a flicker, how do you exercise something you can't move? You identify those with no strength so they can exercise the muscle, but they cannot exercise the muscle.
So, let me put it a different way: I want you to build up your bicep. Here's a dumbbell. Now, do some dumbbell curls, but while you build your bicep, I do not want you to move your bicep.
There is an answer to the salt-on-the-tail dilemma, and I'm getting to one of those answers. And I realized with some coaching, even a flicker could be eventually coached up into something stronger—but try building your bicep muscle in the gym by just “flickering” it.
But I've got a way to maybe do better than that, and I'll get to it in a second.
Bioelectric activity of the pelvic floor and sex
Here's another one: strength and bioelectrical activity of the floor.
There are so many pelvic floor muscle studies out here. And they verified the primary outcomes or level of strength, pelvic floor muscles, and then measured biological activity and sexual function and related it to both stress incontinence and sex.
And what do you think?
As you would expect the people who had weaker muscles and stress incontinence, those with stress incontinence have lower sexual desire and bioelectrical activity with the correlated parameters. Pelvic floor muscle strength of a lower degree correlates with the worse severity of urinary loss, and lower strength correlates with the relationship between the domains of sexual function (all domains of FSFI were involved except for desire).
Training the pelvic floor improves sex
So here's another one. Effects of pelvic floor muscle training on sexual function and satisfaction. In conclusion, pelvic floor muscle training is effectively improving sexual dysfunction and satisfaction and urinary symptoms.
Now, remember the definition of the pelvic floor; when you do a Kegel, remember those female sex muscles I was showing you, ischiocavernosus, superficial and deep transverse peroneal muscle, and bulbospongiosus—those are not the pelvic floor.
A fun female sexercise that you cannot do
Let me demonstrate: if you're a female, right now, close your eyes, concentrate real hard and contract your ischiocavernosus.
Got it?
Now, contract your bulbospongiosus.
If you had trouble thinking about how to do that, well, so would everybody else on the planet. So, doing Kegels does not improve the strength of the female sex muscles!
So what could you do?
How many pelvic floor studies does it take to change the world?
Here’s another study. And you realize these are just samplings; there are so many freaking studies out there about the pelvic floor. Do we really need another one?
Pelvic floor muscle training can improve sexual function, whatever we've known it. We've known it for probably 20, 30, I don't know, when did Dr. Kegel think of this exercise? I'm embarrassed I don't know the history of that, but I think it was about 40 years ago.2
Treatments
Let me swap back over to my picture, and let's think about things to do to treat sexual function by thinking about pelvic muscles.
Okay, so in that study, where they talked about pelvic floor muscles and they could feel either a flicker or nothing at all, in those who had lesser degrees of sexual satisfaction, they were talking about puborectalis; that's what they were palpating. You can see (see video) that your finger goes in; you just feel to the side, you are on puborectalis.
Now, what are some things that can go wrong?
One of them is you can get dyspareunia from the pelvic floor, just like you can get a muscle spasm or a tear or an injury to your back muscles. You can have problems with the pelvic floor.
Imagine a 10-pound baby blasting through that hiatus (looking at video), as they call it. And then what's going to happen to these muscles?
They're not as big as your bicep, they are relatively thin.
And then there's sexual trauma, and then there's just being alive. Your Valsalva when you have a bowel movement, or you ride your bicycle, and you fall, or you climb your cliff, if you're a rock climber woman, or you just slip and fall…and things get injured.
How to see the future of medicine
One way to get some clues about the future of medicine is to look at what they are doing with athletes who make a hundred million dollars per year or race horses that sell for a hundred million dollars.
If you look at that science or at what is provided to these two categories of creatures, you get a clue about the future of medicine—they are testing results in the laboratory of performance and do not have time to wait for the FDA or the AMA.
Even if you're only a high school athlete (not the 100-million-a-year professional), male or female, what did you do when you injured a muscle?
You had physical therapy with massage and vibration and strength building with contraction and relaxation.
You had pressure points, and you had nutrition.
And then, if you had a really bad tear of a muscle, you might immobilize it, or you might do a trigger point injection with corticosteroids.
PRP for the athlete’s muscles
If you are a $100 million quarterback and you tear your thigh muscle, I promise there is one thing that you're going to get that you probably will not see when a mother delivers her baby (unless it’s by one of the obstetricians in our group) And I'm about to show it to you.
Let me put that a different way: there's probably something that you did not get when you delivered your baby, but it's routinely done for professional athletes. So when you injure your muscles delivering a child, in my opinion, you get less use of available technology than what a quarterback gets, even a college quarterback, when they injure a muscle or a tendon.
A study came out this year showing how platelet-rich plasma, because of growth factors that activate pluripotent stem cells to grow new tissue, was used to heal a tendon tear (see references). There are hundreds of studies like this in the sports medicine literature regarding muscle repair.
Let's see if I can pull up a few of them.
I have some representative ones here. I'll throw these in the chat box, too, so you can copy-paste the references.
But what happens if you don't inject PRP and you tear a muscle? I hope this makes you angry; it aggravates me. It should at least aggravate you, or you’re on the wrong call … if you tear a muscle in an elite athlete and then it heals without treatment, there’s fibrosis, there’s loss of strength, there could be loss of function, and the healing time can be prolonged. And if you miss a day of work and you're making $100 million a year, then whoever's paying your salary doesn't like it.
So what do they do?
They inject it with platelet-rich plasma, and studies show that it activates pluripotent stem cells and attenuates the ill effects. You don't have as much fibrosis, you recover your strength faster, and you avoid dysfunction of the muscle that was torn, whether it was the thigh muscle, back muscle, or whatever was injured.
So, back to what we’re talking about, this is just one, and I just copied and pasted other representative studies.
So, one thing that you can do to help with recovery would be just good nutrition. So you have healing.
You could have a massage, which could be pleasant if it is a massage of the pelvic floor. Again, I'm just thinking of analogies between a quarterback for the Dallas Cowboys, a mother who just delivered a child or a mother who delivered a child 20 years ago, and now she's postmenopausal and trying to recover the muscles that were damaged or atrophied some with time.
And those studies have been done: just like a man's bicep atrophies, a woman's pelvic muscles atrophied. Notice I didn't say pelvic floor, pelvic muscles, including transverse perineal muscle, et cetera.
So you could have a physical therapist. You could have cortisone if you had a tear, but you would never do that to a quarterback (weakens the muscle), although it’s still being done for pelvic floor tenderness in regard to dyspareunia in women.
But if you're a quarterback, you would never have that done because you're going to have atrophy. Even in the joints, it's been found that you'll have immediate pain relief if you inject joints with cortisone. But if you watch the joint over a year, you have less joint destruction and even repair with platelet-rich plasma, where you have continued atrophy or even acceleration of osteoporosis and degradation of the joint when you use cortisone.
So why are we still injecting pelvises with cortisone instead of with platelet-rich plasma as is done if it's the muscle of an athlete?
A muscle is a muscle is a muscle. I don't know, but thankfully, you’re on this call, and you can help us change that. So now, what do you do? So you've got a massage, which could be your lover; it could be yourself.
You have trigger point release, and there's a whole science about that out there.
Your pelvic floor physical therapist could do it. But now that you know the anatomy, you can think about what you could say or do, tell your lover to do or do for yourself if you wanted to release tension in the pelvic floor or one of these other muscles like transverse peroneal, superficial or deep or your peroneal body.
So you have trigger point release, or you could do acupuncture.
All these things are done with athletes. You could do vibration; that could be fine. You could also do heat or ice; both of those things are used with the injured athlete.
And then platelet-rich plasma we just talked about. We've been doing it for a decade now, more than a decade, 13 years we've been doing a modified O-Shot® procedure: You still have PRP into the anterior vaginal wall, and into the clitoral body but also into the pelvic muscles, into trigger points.
We have about 1,500 people trained and licensed to do the procedure, but there are 35,000 gynecologists, 20,000 urologists, and 100,000 primary care physicians in the US alone. We need more people who know how to do this, so help us spread the word.
And I think there’s going to be a modification of the O-Shot® that also involves injecting the perineal body with platelet-rich plasma, easy to find, easy to palpate, and that would increase the strength of ischiocavernosus and bulbospongiosus as well as superficial and deep transverse peroneal muscles.
How to turn a flicker into an athletic contraction
Remember we talked about what do you do for the woman who can only flicker or do nothing? How do you train that muscle? She cannot do a Kegel. It's like catching a bird with salt on the tail. If she could move the muscle well, she wouldn’t need to train it, but since she couldn’t move it at all, she couldn’t train it. So she's caught.
Well, that's where your Emsella machine comes in, and there are other devices; but, I think this is probably the Cadillac. And they don't pay me any money to say that. There used to be a vibrator called an intensity, which they called muscle contraction. I've heard it's gone out of production, but even that was not as powerful as an Emsella machine. And I'll show you what it looks like (see links and video).
Enhanced Emsella riding technique for female sex muscle development
But if you're going to use it for sexual function versus urinary incontinence, you should modify the way it's done.
If you go to the O-Shot directory, those who have an Emsella machine, it costs as much as a house, so most people don't have one. But if you find someone who has that icon by their name, then they not only do the O-Shot, but they could combine injecting the pelvic muscles, not just the pelvic floor but the pelvic muscles with PRP along with the O-Shot for sexual function and urinary incontinence. And the Emsella is a Tesla magnet that causes contraction.
So here's their website, but it causes contraction. They're showing contraction of the pelvic floor, but I'm about to show you how to modify the way it's done so that you are contracting not just the pelvic floor but the female sex muscles.
For dyspareunia in the pelvic floor, it could be injecting platelet-rich plasma with a modified O-Shot® procedure by one of our providers combined with pelvic floor physical therapy, good nutrition, and having sex.
I love that part of our aftercare instructions is usually to go have sex. But it should be one of our people so they know how to do the O-Shot® procedure properly. It's not just a shot. People need to know how to make the plasma correctly, how to activate it, where to inject it, and how to inject pain-free.
It's not just throw that needle up in there anywhere. You can hurt people, not damage them, but you can make them hurt. You can cause pain, and if you don’t know what you’re doing and preparing it, you could be unsafe.
So our people know how to keep it safe. And our people offer money back; they’re not going to keep your money if you don't get better. We're not stealing from people and not going to treat you if they don't think they can get you better.
Okay. So, that would be one modification for pelvic floor tenderness with dyspareunia. The other modification for just a super-enhanced sexual enhancement could be improving orgasmic function or arousal, which could be what we already know.
Remember, I don't have to prove this; we know that exercising the pelvis; I just showed you one of literally hundreds of studies showing exercising the pelvis leads to better sexual function.
And then I showed you studies showing that injecting platelet-rich plasma leads to enhanced and improved muscle function, and now you're combining improved muscle function from the exercise physiology research with muscle function with the Emsella, and then you have some good sex and combine that with just good relationships.
Never forget that's an important part of the female. All the rest of the female sexual orgasm system applies. All of it: endocrine, the brain, the spinal cord, the clitoris, the urethral tract, all the components. Some we've covered, and some we haven’t; it all still applies.
But I think with that, unless there are questions, we will call it a day. Let's see what we got. No questions. So, hopefully, that's helpful. Eventually, I'll send the PDF transcript out of this that's edited and tightened up some. And I hope that if you are a patient or a physician, you found something helpful here to make life better.
Have a good day.
Footnotes
- For a little joke, you can tell your friends, another definition of the kiss is the anti juxtaposition of two orbicular oris muscles in the state of contraction. ↩︎
- I looked it up, it was about 60 years ago (in the 1940s) ↩︎
